Polycythemia vera (PV)
Abstract:
Polycythemia vera is a myeloproliferative syndrome with a predominant feature of increased erythropoiesis (increase of the hemoglobin concentration and hematocrit). It usually occurs after the age of 60, however, it can also occur with young patients.
Clinical picture:
The increased hematocrit causes hyperviscosity of the blood. Patients are plethoric. Typical symptoms include headaches, dizziness, lethargy, and pruritus (particularly after bathing or showering). The increased risk for arterial and venous thrombosis is important. If an additional defect of platelet function is present, a tendency toward bleeding could also be present. Hyperuricemia occurs frequently due to the increased cell turnover and can lead to attacks of gout. Splenomegaly is present in 75% of the patients. Unlike chronic myelocytic leukemia, a transition to acute leukemia is less common.
Hematology:
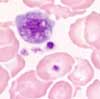 In addition to the increase of hemoglobin and hematocrit values, an increase in the number of leukocytes and platelets is also found in most cases. Basophilia and/or mild eosinophilia is also typical. Since the therapy for polycythemia vera consists of repeated phlebotomy, microcytosis and hypochromia result as a sign of the desired iron deficiency.
In addition to the increase of hemoglobin and hematocrit values, an increase in the number of leukocytes and platelets is also found in most cases. Basophilia and/or mild eosinophilia is also typical. Since the therapy for polycythemia vera consists of repeated phlebotomy, microcytosis and hypochromia result as a sign of the desired iron deficiency.
Bone marrow:
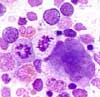 The bone marrow is hypercellular with enhanced erythropoiesis. Megakaryocytopoiesis is also increased. An increase in the basophils and eosinophils is also noticeable. Iron staining usually demonstrates absent iron stores.
The bone marrow is hypercellular with enhanced erythropoiesis. Megakaryocytopoiesis is also increased. An increase in the basophils and eosinophils is also noticeable. Iron staining usually demonstrates absent iron stores.
Table of Contents
 In addition to the increase of hemoglobin and hematocrit values, an increase in the number of leukocytes and platelets is also found in most cases. Basophilia and/or mild eosinophilia is also typical. Since the therapy for polycythemia vera consists of repeated phlebotomy, microcytosis and hypochromia result as a sign of the desired iron deficiency.
In addition to the increase of hemoglobin and hematocrit values, an increase in the number of leukocytes and platelets is also found in most cases. Basophilia and/or mild eosinophilia is also typical. Since the therapy for polycythemia vera consists of repeated phlebotomy, microcytosis and hypochromia result as a sign of the desired iron deficiency. The bone marrow is hypercellular with enhanced erythropoiesis. Megakaryocytopoiesis is also increased. An increase in the basophils and eosinophils is also noticeable. Iron staining usually demonstrates absent iron stores.
The bone marrow is hypercellular with enhanced erythropoiesis. Megakaryocytopoiesis is also increased. An increase in the basophils and eosinophils is also noticeable. Iron staining usually demonstrates absent iron stores.