Parameters of hemolysis
In the investigation of hemolysis, certain tests reflect increased cell destruction and others increased activity of erythropoiesis.
- In the first group are:
bilirubin - LDH - haptoglobin - The tests of the second group are discussed in the unit "Red blood cell parameters". They are:
reticulocyte count - reticulocyte production index - The direct and indirect Coombs test are used to demonstrate anti-erythrocytic autoantibodies.
Bilirubin:
Bilirubin is a degradation product of the heme. The breakdown of hemoglobin generates up to 80% of bilirubin and the breakdown of myoglobin generates the remaining 20%. Bilirubin is glucuronated in the liver and immediately excreted in the bile. The glucuronated form is also called conjugated or direct and the non-glucuronated form is also called unconjugated or indirect. In hemolytic disease, unconjugated bilirubin is increased. Unconjugated bilirubin is a sensitive but nonspecific test.
Normal range: Total Bilirubin
µmol/L, direct (conjugated) Bilirubin
µmol/L.
Lactate dehydrogenase
Lactate dehydrogenase (LDH) is an enzyme that is present in many cells. Erythrocytes have especially high amounts of LDH. Therefore, LDH is increased in hemolysis. Similar to the unconjugated bilirubin, LDH is a sensitive but nonspecific test.
Normal range:
IU/L.
Haptoglobin
Haptoglobin binds free hemoglobin and is immediately eliminated in the liver. Haptoglobin is produced in the liver and therefore decreased in disorders of liver function. Being an acute phase protein, haptoglobin is increased in inflammatory states. As soon as degradation of haptoglobin is higher than its production its level decreases.
Typically, haptoglobin is decreased in intravascular hemolysis, e.g. acute autoimmune hemolytic anemia, microangiopathic hemolytic anemia or infectious hemolysis (Malaria). In extravascular hemolysis such as e.g. ineffective erythropoiesis, subacute immune hemolysis or hypersplenism, haptoglobin is only decreased if degradation capacity of the reticuloendothelial system is surpassed and free hemoglobin becomes present intravascularly. In concurrent inflammation, haptoglobin can be false-normal.
Haptoglobin too is a sensitive but nonspecific test for hemolysis.
Normal range:
-
g/L.
Direct antiglobulin test (DAT or direct Coombs test)

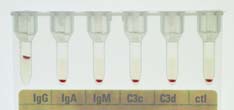
With the DAT, antibodies and complement components fixed in vivo to the surface of red blood cells can be demonstrated. The basic principle of the DAT is the agglutination of patient erythrocytes. This is induced be adding antiglobulin serum (Coombs serum), which can be polyspecific (Anti-IgG and Anti-complement; upper image, gel test) or for further differentiation monospecific (Anti-IgG1-4, -IgA, -IgM, -C3c, -C3d; lower image).
A positive DAT allows only the conclusion that immunoglobulin and/or complement are fixed to the surface of the patient erythrocytes (up to 3-15% of in-patients and 1/1000 to 1/14 000 of healthy blood donors have a positive DAT). Therefore, the interpretation depends also on clinical findings and other lab examinations. A positive DAT is mainly found in autoimmune hemolytic anemia, drug induced immune hemolytic anemia, hemolytic transfusion reactions and in hemolytic disease of the newborn.
Indirect antiglobulin test (IAT or indirect Coombs test)
With the IAT the presence of free anti-erythrocytic autoantibodies in the serum is detected. In contrast to the DAT, the patient's serum is incubated with normal erythrocytes. Then the indirect Coombs test is performed and interpreted like the direct Coombs test.
A positive IAT indicates, that antibodies against known antigens on the normal erythrocytes are present. Dies test is used for antibody screening or cross-matching before a blood transfusion, for antibody screening in pregnancy, for demonstration of special blood group characteristics or for the screening for free antibodies if the DAT is positive.