Red blood cell parameters
Hemoglobin - Hematocrit - Erythrocyte count - Erythrocyte indices - RDW - Reticulocyte count - Reticulocyte production index - Reticulocyte counting by flow cytometry
Hemoglobin:
Hemoglobin concentration is a more precise term than hemoglobin since the amount of hemoglobin per unit volume (L) is measured. The hemoglobin concentration can vary considerably depending on the patient's state of hydration. Hemoglobin is usually measured spectrophotometrically.
Normal range: Men
-
g/L, women
-
g/L.
High leukocyte counts can interfere with the measurement of hemoglobin due to clouding. Therefore, if very high leukocyte counts are present (limits differ among the automated cell counters) blood has to be lysed manually and centrifuged. The measurement of hemoglobin is done manually in the leukocyte-free supernatant.
Hematocrit:
Hematocrit corresponds to the percentage of the cells in the blood volume. This value is expressed as a fraction (liter/liter) or in percent. Hematocrit is measured by the direct reading of a blood-filled tube that has previously been centrifuged, or it is calculated from the hemoglobin by an electronic cell counting device.
Normal range: Men
-
L/L or
-
%, women
-
L/L or
-
%. The general standard value is 0.45 L/L or 45%.
Erythrocyte or red cell count:
The erythrocyte count deals with red cell concentration per liter. In the past, the measurement of erythrocytes was done microscopically with a counting chamber. Nowadays, automated cell counters are used since they deliver far more precise counts due to the high number of erythrocytes counted.
Normal range: Men - x 1012/L, women - x 1012/L.
Erythrocyte indices:
Erythrocyte indices are derived from the values of hemoglobin (Hb), hematocrit (Hc) and the erythrocyte count (Ec). They reflect erythrocyte volume and hemoglobin concentration in the erythrocyte. Historically, hemoglobin, hematocrit and red cell count were measured and consequently MCV, MCH and MCHC calculated. Today's automated cell counters measure hemoglobin, MCV and red cell count and derive from these data hematocrit, MCH and MCHC.
| Calculation: | MCV (fl) = | Hc (L/L)
Ec |
x 103 | or | Hc (%)
Ec |
x 10 |
|---|---|---|---|---|---|---|
| Example: |
MCV (fl) =
|
0.45 L/L
5.0 x 1012/L |
x 103 | = 90 fl | ||
| Normal range: - fl (femtoliter = 10-15L). | ||||||
| Calculation: | MCH (pg) = | Hb
Ec |
||
|---|---|---|---|---|
| Example: | MCH (pg) = | 150 g/L
5.0 x 1012/L |
= | 30 pg |
| Normal range: - pg (picogram = 10-12g). | ||||
| Calculation: | MCHC (g/l) = | Hb
Hc (L/L) |
or | Hb
Hc (%) |
x 100 |
|---|---|---|---|---|---|
| Example: | MCHC (g/l) = | 150 g/L
0.45 L/L |
= 333 g/L | ||
| Normal range: - g/L. | |||||
Erythrocyte indices allow anemias to be defined more precisely. Therefore, based on the MCV, anemias can be classified as microcytic (iron deficiency anemia, thalassemia), normocytic (anemia of chronic disorders, anemia of renal disease), and macrocytic (megaloblastic anemia). The MCH classifies hypochromic (iron deficiency anemia, thalassemia) and normochromic (anemia of chronic disorders, anemia of renal disease). Usually, although not always, the terms microcytic/hypochromic, normocytic/normochromic and macrocytic/hyperchromic are paired.
RDW = Red cell distribution width
The RDW is a parameter for the size variability of erythrocytes. Thus, it is a numeric expression for anisocytosis. It is calculated by automated cell counters using the following formula:
|
RDW = |
standard deviation of erythrocyte volume
MCV |
x 100 |
|---|---|---|
|
Normal range: 11.5 - 14.5 %. |
||
Together with the MCV, the RDW provides diagnostic clues if anemia is present.
| Normal RDW | Increased RDW | |
|---|---|---|
| Normocytic |
Acute hemolysis |
Autoimmune hemolytic anemia |
| Microcytic |
Heterozygous thalassemias, |
Iron deficiency anemia |
| Macrocytic |
Myelodysplastic syndromes |
Myelodysplastic syndromes |
The RDW is helpful for the differentiation between iron deficiency anemia and anemia of chronic disorders.
| RDW | MCV | |
|---|---|---|
| iron deficiency anemia |
increased |
normal or decreased |
| anemia of chronic disorders |
normal |
normal or decreased |
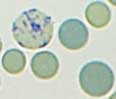
Since reticulocytes are not recognized by Wright staining, they must be made visible by the so-called supravital staining (staining of a non-fixed film). In this staining, the reticulocytes' net-like precipitates are recognizable. The reticulocytes are counted by microscopy in relation to the erythrocytes. The normal value is 0.5 to 2% of the erythrocytes. This value corresponds to the observation that the reticulocytes need around 1-2 days (approximately one hundredth of the erythrocytes' life span) to mature into erythrocytes. In absolute numbers, the normal range is - x 109/L.
Reticulocyte production index (RPI)
The younger the reticulocytes are when they are released from the bone marrow, the longer the maturation time and the longer the period of time in which they can be detected in the peripheral blood. Since this leads to falsely high values, it is recommended that a correction be done. The normal value of the RPI is 1 (one). A result below 1 signifies that the production rate is to low in comparison for the degree of anemia (hyporegenerative anemia).
| Calculation: | Reticulocyte production index | = | Reticulocyte count in %
F (taken from table below) |
|
|---|---|---|---|---|
| Example: | Reticulocyte production index in a Hematocrit of 0.20 L/L |
= | 7.5%
5.1 |
= 1.47 |
| Hc | F | Hc | F | Hc | F | Hc | F |
|---|---|---|---|---|---|---|---|
| 0.10 | 12.4 | 0.19 | 5.5 | 0.28 | 3.0 | 0.37 | 1.7 |
| 0.11 | 11.0 | 0.20 | 5.1 | 0.29 | 2.8 | 0.38 | 1.6 |
| 0.12 | 9.9 | 0.21 | 4.7 | 0.30 | 2.6 | 0.39 | 1.5 |
| 0.13 | 9.0 | 0.22 | 4.4 | 0.31 | 2.5 | 0.40 | 1.4 |
| 0.14 | 8.2 | 0.23 | 4.1 | 0.32 | 2.3 | 0.41 | 1.3 |
| 0.15 | 7.5 | 0.24 | 3.8 | 0.33 | 2.2 | 0.42 | 1.2 |
| 0.16 | 6.9 | 0.25 | 3.6 | 0.34 | 2.1 | 0.43 | 1.2 |
| 0.17 | 6.4 | 0.26 | 3.4 | 0.35 | 1.9 | 0.44 | 1.1 |
| 0.18 | 5.9 | 0.27 | 3.2 | 0.36 | 1.8 | 0.45 | 1.0 |
Reticulocyte counting by flow cytometry
In this method, the RNA of reticulocytes is stained with a fluorescent dye. The measurement of the fluorescent intensity allows categorization of reticulocytes into three groups:
1. LFR = low fluorescence ratio (= little RNA = mature)
2. MFR = medium fluorescence ratio (= much RNA = immature)
3. HFR = high fluorescence ratio (= very much RNA = very immature)
MFR and HFR together result in the IFR (immature reticulocyte fraction). The IFR is a parameter that gives similar information on the activity of the erythropoiesis as the reticulocyte production index.